Ref : https://ou.edu/content/publicaffairs/archives/OUTeamDevelopsNewAntibioticFormulationtoFightMRSAandOtherAntibioticResistantBacteria.html
Wednesday, November 2, 2016
New drug that combines methicillin with polymer BPEI can combat MRSA
Ref : https://ou.edu/content/publicaffairs/archives/OUTeamDevelopsNewAntibioticFormulationtoFightMRSAandOtherAntibioticResistantBacteria.html
Friday, October 28, 2016
Natural product darwinolide may help combat fatal MRSA infection

Tuesday, January 24, 2017
New experimental antibiotic can help combat MRSA infections
"Current standard-of-care drugs for the treatment of MRSA infections are limited," said Pilch. "Furthermore, resistance to these drugs is on the rise, and their clinical effectiveness is likely to diminish in the future."
Ref : http://aac.asm.org/content/59/8/4845.full?sid=949e5603-f4b2-4eec-8e5f-f79d0c758e44
Thursday, June 4, 2015
Two common antibiotic treatments equally effective against MRSA skin infections
Researchers funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, have found that two common antibiotic treatments work equally well against bacterial skin infections caused by methicillin-resistant Staphylococcus aureus (MRSA) acquired outside of hospital settings. Known as community-associated MRSA, or CA-MRSA, these skin infections have been reported in athletes, daycare-age children, students, military personnel and prison inmates, among others, and can lead to hospitalization, surgical procedures, bacteria in the blood, and in severe cases, death.
Wednesday, January 20, 2016
Novel class of antimicrobials could be effective in fighting drug-resistant MRSA infection
Thursday, January 21, 2016
Innovative compound with anti-MRSA qualities may help develop new class of antibiotics
As today’s infections develop increasing resistance to the antibiotics of the past, there is an urgent need for researchers to develop new therapeutics. Without this action, we are seriously at risk of entering a post-antibiotic world where common and traditionally minor infections could once again prove fatal. Discovering the antibacterial properties of our lead compound, the highly active quinoline thiourea, at Maynooth University is a significant first step. With further research and development, it has the potential to pave the way for a new class of antibiotic.
Thursday, December 1, 2016
Theravance Biopharma Announces FDA Approval of Expanded Label for Vibativ (telavancin)
Expanded Vibativ Label Data
- In the all-treated cSSSI patient population with baseline S. aureus bacteremia in the ATLAS I and II trials, clinical cure rates at test-of-cure were 57.1% for Vibativ-treated patients vs. 54.6% for vancomycin-treated patients.
- In the HABP/VABP patient population with at least one Gram-positive respiratory pathogen at baseline who had concurrent S. aureus bacteremia in the ATTAIN I and II trials, the 28-day all-cause mortality rate was 40.0% for Vibativ-treated patients vs. 39.5% for vancomycin-treated patients.
Thursday, October 2, 2014
Scripps Research Institute Chemists Modify Antibiotic to Vanquish Resistant Bacteria
Wednesday, September 25, 2024
FDA Approves Zevtera (ceftobiprole medocaril sodium) for Bacteremia, Skin and Skin Structure Infections, and Pneumonia
Basilea Pharmaceutica Ltd, Allschwil (SIX: BSLN), a commercial-stage biopharmaceutical company committed to meeting the needs of patients with severe bacterial and fungal infections, announced today that the US Food and Drug Administration (FDA) approved Zevtera® (ceftobiprole medocaril sodium for injection), for the treatment of adult patients with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including those with right-sided infective endocarditis, and adult patients with acute bacterial skin and skin structure infections (ABSSSI) and for adult and pediatric patients (3 months to less than 18 years old) with community-acquired bacterial pneumonia (CABP).
David Veitch, Chief Executive Officer of Basilea, said: “We are excited with the US approval of Zevtera. The positive decision by the FDA is a key milestone towards bringing Zevtera to patients in the US. Zevtera has 10 years of market exclusivity from the date of approval and we believe the US provides the most important global commercial opportunity for the brand.”
Dr. Marc Engelhardt, Chief Medical Officer of Basilea, stated: “We are very pleased that the FDA approved Zevtera for all three indications that were submitted with the NDA, including a pediatric labelling. This approval is a landmark for ceftobiprole and reflects its broad clinical utility. The indication in adult patients with Staphylococcus aureus bacteremia, including those with right-sided infective endocarditis, caused by methicillin-susceptible and methicillin-resistant isolates, MSSA and MRSA, addresses a real medical need, as current treatment options are limited.”
The New Drug Application (NDA) was supported by clinical efficacy and safety data from the phase 3 studies ERADICATE (SAB)1 and TARGET (ABSSSI),2 and a phase 3 study in CABP.3 The ERADICATE study was the largest double-blind randomized registrational study conducted for a new antibiotic treatment in SAB.
Vance G. Fowler, Jr., M.D., Professor in the Departments of Medicine and Molecular Genetics & Microbiology at the Duke University School of Medicine and academic lead investigator of the ERADICATE study, commented: “Complicated Staphylococcus aureus infections have a high mortality rate and are associated with substantial morbidity. We need more options for treating these infections, especially if MRSA is involved.”
Thomas Holland, M.D., Associate Professor in the Department of Medicine at the Duke University School of Medicine and chair of the data review committee of the ERADICATE study, added: “There is a high medical need in Staphylococcus aureus bacteremia, therefore, the first approval of a therapy for this indication in over 15 years is highly welcome.”
Adesh Kaul, Chief Financial Officer of Basilea, added: “As we were moving towards completion of the regulatory review, especially with increasing visibility on the expected label, the external interest for commercial partnering increased. Whilst our initial goal was to have announced a commercial partnership by the time of approval of Zevtera in the US, in order to explore fully all potential partnering opportunities, we now expect to complete the process around mid-year. In parallel, we are also taking preparatory steps to shorten the launch timelines, once we have entered into a commercialization partnership.”
Basilea’s phase 3 program for ceftobiprole is funded in part with federal funds from the US Department of Health and Human Services (HHS); Administration for Strategic Preparedness and Response (ASPR); Biomedical Advanced Research and Development Authority (BARDA), under contract number HHSO100201600002C. Through this partnership, Basilea has been awarded approximately USD 112 million, or approximately 75 percent of the costs related to the SAB and ABSSSI phase 3 studies, regulatory activities and non-clinical work.
About Zevtera® (ceftobiprole medocaril sodium for injection)
Ceftobiprole, the active moiety of the prodrug ceftobiprole medocaril, is an advanced generation cephalosporin antibiotic for intravenous administration, with rapid bactericidal activity against a wide range of Gram-positive bacteria, such as Staphylococcus aureus, including methicillin-resistant strains (MRSA), and Gram-negative bacteria.4 In several countries in Europe and beyond, the brand is currently approved and marketed as Zevtera® and Mabelio® for the treatment of adult patients with hospital-acquired bacterial pneumonia (HABP), excluding ventilator-associated bacterial pneumonia (VABP), and for the treatment of community-acquired bacterial pneumonia (CABP). Basilea has entered into license and distribution agreements covering more than 80 countries. In the United States, Zevtera is indicated for the treatment of adult patients with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including right-sided infective endocarditis, and adult patients with acute bacterial skin and skin structure infections (ABSSSI) and for adult and pediatric patients (3 months to less than 18 years old) with community-acquired bacterial pneumonia (CABP).
Tuesday, April 21, 2009
White light-activated antibacterial coating-a new weapon against superbugs ?
Cutting rates of healthcare associated infections (HCAIs) such as Methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile (C.Diff) is a key priority for healthcare professionals. Recently in my earlier blog, I did mention that they were able to culture many bacterii from the cell phones of the health workers !.
Thogh govts., are taking many intiatives with sterlisation of the instrements, the rooms still something has to be done. But this is really something interesting which I read recently and want to share with...
Miss Zoie Aiken and her colleagues presented the work at the Society for General Microbiology meeting in Harrogate on 31 March, 2009. The veneer-like surface, made of titanium dioxide with added nitrogen. When it is activated by white light, similar to those used in hospital wards and operating theatres, it produced a decrease in the number of bacteria surviving on the test surface. Really interesting and the basis for this research is that "Titanium dioxide based coatings can kill bacteria after activation with UV light. The addition of nitrogen to these coatings enables photons available in visible light to be utilised to activate the surface and kill bacteria".
The following are the conclusions :
1. the activity of the coating is assessed against a range of different bacteria such as MRSA and other organisms which are known to cause infections in hospitals. At present researchers claim that the coating is active against Escherichia coli. However, E. coli is more difficult to kill than bacteria from the Staphylococcus group which includes MRSA and the results to date are encouraging.
2. the coating has currently been applied onto glass using a method called APCVD (atmospheric pressure chemical vapour deposition and the researchers want to try out plastic.
Once again congrats and best wishes for further research..
Source : http://www.sgm.ac.uk/
Thursday, November 6, 2014
Scientists develop new drug as alternative to antibiotics
In a small patient trial, the drug was shown to be effective at eradicating the superbug Methicillin-resistant Staphylococcus aureus (MRSA).
Monday, April 12, 2010
2-aminoimidazole/triazole conjugate re-sensitizes multi-drug resistant strains of bacteria to the effects of conventional antibiotics...
Monday, November 23, 2015
Tamoxifen drug clears MRSA, reduces mortality
In continuation of my update on Tamoxifen

Thursday, April 8, 2021
FDA Approves Kimyrsa (oritavancin) for the Treatment of Adult Patients with Acute Bacterial Skin and Skin Structure Infections (ABSSSI)
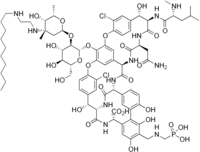
Melinta Therapeutics, LLC (Melinta), a commercial-stage company focused on the development and commercialization of novel antibiotics, today announced that the U.S. Food and Drug Administration (FDA) has approved Kimyrsa (oritavancin) for the treatment of adult patients with acute bacterial skin and skin structure infections (ABSSSI) caused by susceptible isolates of designated Gram-positive microorganisms, including methicillin-resistant Staphylococcus aureus (MRSA). Kimyrsa is a lipoglycopeptide antibiotic that delivers a complete course of therapy for ABSSSI in a single, one hour 1,200 mg infusion.
“The approval of Kimyrsa demonstrates Melinta’s commitment to provide innovative therapies to patients with acute and life-threatening illnesses,” said Christine Ann Miller, President and Chief Executive Officer of Melinta. “We have responded to the requests of the medical community to provide an oritavancin product with a shorter infusion time. We believe that with the approval of Kimyrsa and product availability this summer, physicians and patients will now have a compelling new one-dose alternative to the current standard of multi-dose regimens for ABSSSI.”
ABSSSI affect approximately 14 million patients in the U.S. each year, are responsible for over 3 million visits to the Emergency Room annually and represent the 8th most common cause of Emergency Department hospital admissions1,2. ABSSSI cost U.S. hospitals $4 billion each year, with a 4.1-day average length of stay for hospitalized ABSSSI patients.2
“Kimyrsa is an important new treatment option that will provide clinicians with additional flexibility to treat ABSSSI patients in multiple care settings, without the need for hospitalization,” said Andrew Dold, D.O., member of a private infectious disease practice covering the Greater Atlanta Region. “Single-dose, long-acting antibiotics, such as Kimyrsa, may be especially beneficial for patients who lack the support or resources to adhere to multiple intravenous administrations.”
The efficacy and safety of Kimyrsa were established in the SOLO clinical trials with another oritavancin product, Orbactiv. The SOLO trials were randomized, double-blind, multicenter studies that evaluated a single 1,200 mg IV dose of oritavancin against twice-daily vancomycin for the treatment of ABSSSI in 1,987 adult patients and assessed one of the largest subsets of documented MRSA infection (405 patients). These trials demonstrated that 1,200 mg one-dose IV oritavancin infusion was as effective as 7-to-10 days of twice-daily vancomycin (1 g or 15 mg/kg) for the primary and secondary endpoints. Kimyrsa approval is based on the results of an open-label, multi-center, pharmacokinetics study, which compared Kimyrsa administered over 1 hour (N=50) to Orbactiv administered over 3 hours (N=52) for the treatment of adult patients with ABSSSI.
Michael Waters, M.D. and lead investigator in the PK clinical trial stated, “Kimyrsa was shown to be comparable to Orbactiv with a favorable safety profile. I’m pleased that these outcomes support the approval of Kimyrsa to provide oritavancin with a shorter infusion time and lower infusion volume. With these features, Kimyrsa can further enhance the treatment experience for the patient and efficiency of administration in clinical practice.”
Wednesday, May 25, 2011
Linezolid more effective than vancomycin in treating ventilated patients with MRSA pneumonia: Study
Linezolid more effective than vancomycin in treating ventilated patients with MRSA pneumonia: Study
Monday, May 24, 2010
Thursday, February 21, 2013
New Antibiotic May Treat Skin Infections in Shorter Time - Drugs.com MedNews
Monday, May 31, 2010
Plectasin - a new weapon against highly resistant microbes ?..
In this process, plectasin behaves like a thief which steals the stones off a mason. 'It binds to a cell-wall building block called lipid II and thus prevents it from being incorporated ,' Professor Sahl explains. 'However, bacteria cannot live without a cell wall.' It comes as no surprise that the most famous antibiotic penicillin also inhibits cell-wall synthesis...
Wednesday, June 11, 2014
Promising discovery in fight against antibiotic-resistant bacteria .....
Monday, April 25, 2016
Allergan Announces FDA Approval of Updated Label for New Dosing Regimen for Dalvance (dalbavancin)








